The Leadership group for this workstream includes two transplant surgeons from across the region, a lead Nephrologist and a QI Manager. The group has established good working links across all specialities within the region. The group has also established excellent communication between all Renal sites in the North West.
The image below shows that the transplant workstream has identified completed a thorough assessment of what is needed to enlist and maintain a patient onto to transplant list. As illustrated a bottleneck of services required has been identified within the region and work is now underway to address this. Details of the works commenced and planned are located within the accordions below.
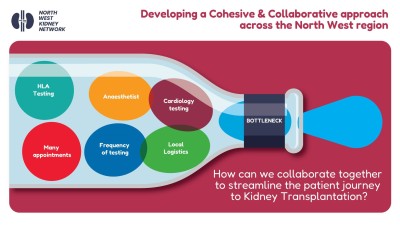
There has been a strong focus on the identification of bottlenecks that can affect why patients do not get listed for transplant in a timely manner. This workstream has nearly completed a NW Pre Transplant assessment and investigations guideline. This guideline will set out the rationale for guidance with a strong focus on both symptomatic and asymptomatic patients.
This work is being led by the two surgeons within the workstream. Looking at current pathways within the 2 transplanting sites in the NW.
This workstream has been trying to establish a peer support network for the past 12 months. Access to transplantation faces two major hurdles: limited organ availability and inefficient referral networks. Together, these barriers can lead to avoidable excess mortality among individuals with end-stage organ disease.
- People, families and communities can play a key role in managing their own health and wellbeing. Peer support involves people sharing knowledge, experience or practical help with each other. Many voluntary and community groups encourage peer support. Health and social care commissioners are beginning to recognise the potential benefits. Peer support can be offered in many ways, either in person, online or by telephone.
- There is much evidence that peer support can help people feel more knowledgeable, confident, happy and less isolated and alone. Patients with kidney disease can often learn and gain support from their fellow patients, and peer support is becoming an increasing area of practice in health care. One of the distinct benefits of peer support derive from the fact that only another renal patient can share the personal experience of living with kidney disease.
- Limited information and health literacy especially among ethnic minorities can have a negative effect on transplant rates. It is commonly seen that patients and/or families of ethnic minorities refuse transplantation or donation due to misunderstandings and uncertainty regarding the unknown.
- A need to recruit black, Asian and minority ethnic community champions throughout the peer support process.
In October 2024 the NW completed its first training day in peer support at Salford NCA. This was well attended, and the next steps are to continue to roll this out across the whole NW area.
We are very near to completing the Transplant data dashboard for the NW. We are awaiting final checks from data control before showcasing this work. This will tell a story of transplantation across the NW with up to date figures being transplanted and those awaiting transplant.
This is a collaborative piece of work currently being run alongside KQIP. We wish to highlight and focus on the patient and clinician perspective of what is required at the pre transplant annual review. There can be a number of implications for waiting a long time for transplant. There could be psychological stress and uncertainty for patients. The aim for this work is to try to marry the clinician tests and patient expectation at the annual review.
The advantages of a good annual review are plenty, a few examples are below:
- A reduction in the suspension on waiting list
- Reduces unnecessary investigations
- Reduces cancellation on the day of surgery
- Improves patient outcomes and knowledge base
The Transplant workstream is constantly reviewing the process of post-transplant care. We have started to review waiting times to repatriate patients back to their home base unit following transplant.
One aim is to improve coordination between hospitals regarding post-transplant follow-up.
- Develop a consensus on improving post-transplant follow-up, including investigations and monitoring such as CMV/BK screening, immunological surveillance, urine PCR, Hba1c, metabolic tests, and cancer surveillance.
- Repatriation: Discuss general views, benefits, risks, logistical support, minimum paperwork needed and agreed time frame.
- Approaches for providing personalized immunosuppression based on immunological and infection risk profiles.
- Regional data: Detailed data on post-transplant events such as diabetes, rejection, metabolic CV events, and infection is lacking.
- Agreement on the pathway for patients with Delayed Graft Function and Primary Non Function
- Consensus on immunological surveillance
- Local experience in managing refractory rejections, access to ATG and PLEX, and GN recurrence.
- The Setting up of a regional infectious disease clinic (virtual).
- A review of incidents, coroners, deaths, and causes of admissions.
- Any other issues the team would like to discuss can also be included in the working group discussions.